Angioplasty and Stent Placement for the Heart
What is angioplasty?
Angioplasty, also called percutaneous coronary intervention (PCI), is a procedure used to open blocked coronary arteries (caused by coronary artery disease) and restore blood flow to the heart muscle without open-heart surgery.
For angioplasty, a special catheter (a long, thin, hollow tube) is inserted into a blood vessel and guided to the blocked coronary artery. The catheter has a tiny balloon at its tip. Once the catheter is in place, the balloon is inflated at the narrowed area of the coronary artery. This presses the fatty tissue against the sides of the artery making more room for blood flow.
The use of fluoroscopy (a special type of X-ray that’s like an X-ray “movie”) helps the doctor find the blockages in the coronary arteries as a contrast dye moves through the arteries.
The doctor may determine that another type of procedure is necessary. This may include the use of atherectomy (removal of plaque) at the site of the narrowing of the artery. In atherectomy, there may be tiny blades on a balloon or a rotating tip at the end of the catheter. When the catheter reaches the narrowed spot in the artery, the plaque is broken up or cut away to open the artery.
Stents
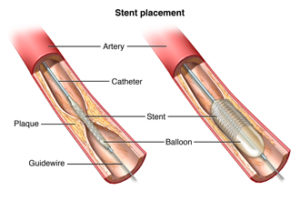
Coronary stents are now used in nearly all angioplasty procedures. A stent is a tiny, expandable metal mesh coil that is put into the newly-opened area of the artery to help keep the artery from narrowing or closing again.
Once the stent has been placed, tissue will begin to form over it within a few days after the procedure. The stent will be completely covered by scar tissue within a month or so. Medication must be taken to decrease the “stickiness” of platelets (special blood cells that clump together to stop bleeding), to keep blood clots from forming inside the stent. Your doctor will give specific instructions on which medications need to be taken and for how long.
Some stents are coated with medication to prevent the formation of too much scar tissue inside the stent. These stents, called drug-eluting stents, or DES, release medication within the blood vessel that inhibits the overgrowth of tissue within the stent, and helps deter re- narrowing of the blood vessel.
Because stents can become blocked, it is important for you to talk with your doctor about what you need to do if you have chest pain after a stent placement.
If scar tissue does form inside the stent, a repeat procedure may be needed, either with balloon angioplasty or with a second stent. In some cases, radiation therapy may be given through a catheter placed near the scar tissue to stop the growth of scar tissue and open up the vessel.
Why might I need angioplasty?
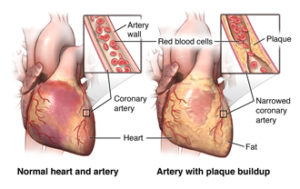 Angioplasty is done to restore coronary artery blood flow when the narrowed artery is in a location that can be reached in this manner. Not all coronary artery disease (CAD) can be treated with angioplasty. Your doctor will decide the best way to treat your CAD based on your circumstances.
Angioplasty is done to restore coronary artery blood flow when the narrowed artery is in a location that can be reached in this manner. Not all coronary artery disease (CAD) can be treated with angioplasty. Your doctor will decide the best way to treat your CAD based on your circumstances.
What are the risks of angioplasty?
Possible risks associated with angioplasty, stenting, atherectomy, and related procedures include, but are not limited to:
- Bleeding at the site where the catheter is put into the body (usually the groin, wrist, or arm)
- Blood clot or damage to the blood vessel from the catheter
- Blood clot within the treated blood vessel
- Infection at the catheter insertion site
- Arrhythmias (abnormal heart rhythms)
- Heart attack
- Stroke
- Chest pain or discomfort
- Rupture of the coronary artery or complete closing of the coronary artery, requiring open-heart surgery
- Allergic reaction to the contrast dye used
You may want to ask your doctor about the amount of radiation used during the procedure and the risks related to your particular situation. It is a good idea to keep a record of your radiation exposure, such as previous scans and other types of X-rays, so that you can inform your doctor. Risks associated with radiation exposure may be related to the cumulative number of X-rays and/or treatments over a long period.
For some people, having to lie still on the procedure table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
How do I get ready for angioplasty?
- Your doctor will explain the procedure to you and you can ask questions.
- You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if anything is not clear.
- Tell your doctor if you have ever had a reaction to any contrast dye, or if you are allergic to iodine.
- Tell your doctor if you are sensitive to or are allergic to any medications, latex, tape, and anesthetic agents (local and general).
- You will need to fast (not eat or drink) for a certain period prior to the procedure. Your doctor will tell you how long to fast, whether for a few hours or overnight.
- If you are pregnant or think you may be pregnant, tell your doctor. Radiation exposure during pregnancy may lead to birth defects.
- Tell your doctor if you have any body piercings on your chest and/or abdomen (belly).
- Tell your doctor of all medications (prescription and over-the-counter), vitamins, herbs, and supplements that you are taking.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant or antiplatelet (blood-thinning) medications, aspirin, or other medications that affect blood clotting. You may need to stop some of these medications prior to the procedure. However, for planned angioplasty procedures, your doctor may want you to continue taking aspirin and antiplatelet medications, so be sure to ask.
- Your doctor may request a blood test prior to the procedure to determine how long it takes your blood to clot. Other blood tests may be done as well.
- Tell your doctor if you have a pacemaker.
- You may get a sedative prior to the procedure to help you relax.
- Based on your medical condition, your doctor may request other specific preparation.
What happens during angioplasty?
Angioplasty may be done as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor’s practices.
Generally, angioplasty follows this process:
- You will be asked to remove any jewelry or other objects that may interfere with the procedure. You may wear your dentures or hearing aid if you use either of these.
- You will be asked to remove your clothing and will be given a gown to wear.
- You will be asked to empty your bladder prior to the procedure.
- If there is a lot of hair at the area of the catheter insertion (often the groin area), the hair may be shaved off.
- An intravenous (IV) line will be started in your hand or arm prior to the procedure. It will be used for injection of medication and to administer IV fluids, if needed.
- You will be placed on your back on the procedure table.
- You will be connected to an electrocardiogram (ECG) monitor that records the electrical activity of your heart and monitors your heart rate using electrodes that stick to your skin. Your vital signs (heart rate, blood pressure, breathing rate, and oxygen level) will be monitored during the procedure.
- There will be several monitor screens in the room, showing your vital signs, the images of the catheter being moved through your body into your heart, and the structures of your heart as the dye is injected.
- You will get a sedative in your IV to help you relax. However, you will likely stay awake during the procedure.
- Your pulses below the catheter insertion site will be checked and marked so that the circulation to the limb below the site can easily be checked during and after the procedure.
- A local anesthetic will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected.
- Once the local anesthetic has taken effect, a sheath, or introducer, will be put into the blood vessel (often at the groin). This is a plastic tube through which the catheter will be threaded into the blood vessel and advanced into the heart.
- The catheter will be threaded through the sheath into the blood vessel. The doctor will advance the catheter through the aorta into the heart. Fluoroscopy (an X-ray “movie”) will be used to help see the catheter advance into the heart.
- The catheter will be threaded into the coronary arteries. Once the catheter is in place, contrast dye will be injected through the catheter into your coronary arteries in order to see the narrowed area(s). You may feel some effects when the contrast dye is injected into the IV line. These effects include a flushing sensation, a salty or metallic taste in the mouth, and/or a brief headache. These effects usually last only a few moments.
- You should notify the doctor if you feel any breathing difficulties, sweating, numbness, itching, nausea and/or vomiting, chills, or heart palpitations.
- After the contrast dye is injected, a series of rapid X-ray images of the heart and coronary arteries will be taken. You may be asked to take in a deep breath and hold it for a few seconds during this time.
- When the doctor locates the narrowed artery, the catheter will be advanced to that location and the balloon will be inflated to open the artery. You may have some chest pain or discomfort at this point because the blood flow is temporarily blocked by the inflated balloon. Any chest discomfort or pain should go away when the balloon is deflated. However, if you notice any continued discomfort or pain, such as chest pain, neck or jaw pain, back pain, arm pain, shortness of breath, or breathing difficulty, tell your doctor right away.
- The doctor may inflate and deflate the balloon several times. The decision may be made at this point to put in a stent to keep the artery open. In some cases, the stent may be put into the artery before the balloon is inflated. Then the inflation of the balloon will open the artery and fully expand the stent.
- The doctor will take measurements, pictures, or angiograms after the artery has been opened. Once it has been determined that the artery is opened sufficiently, the catheter will be removed.
- The sheath or introducer is taken out and the insertion site may be closed with a closure device that uses collagen to seal the opening in the artery, by the use of sutures, or by applying manual pressure over the area to keep the blood vessel from bleeding. Your doctor will decide which method is best for you.
- If a closure device is used, a sterile dressing will be applied to the site. If manual pressure is used, the doctor (or an assistant) will hold pressure on the insertion site so that a clot will form. Once the bleeding has stopped, a very tight bandage will be placed on the site. A small sandbag or other type of weight may be placed on top of the bandage for additional pressure on the site, especially if the site is in the groin.
- Staff will help you slide from the table onto a stretcher so that you can be taken to the recovery area. NOTE: If the insertion was in the groin, you will not be allowed to bend your leg for several hours.If the insertion site was in the arm, your arm will be kept elevated on pillows and kept straight by placing your arm in an arm guard (a plastic arm board designed to immobilize the elbow joint). In addition, a plastic band (that works like a belt around the waist) may be secured around your arm near the insertion site. The band will be loosened at given intervals and then removed when your doctor decides the pressure is no longer needed.
What happens after angioplasty?
In the hospital
After the procedure, you may be taken to the recovery room for observation or returned to your hospital room. You will stay flat in bed for several hours after the procedure. A nurse will monitor your vital signs, the insertion site, and circulation/sensation in the affected leg or arm.
Tell your nurse right away if you feel any chest pain or tightness, or any other pain, as well as any feelings of warmth, bleeding, or pain at the insertion site.
Bed rest may vary from 2 to 6 hours depending on your specific condition. If your doctor placed a closure device, your bed rest may be shorter.
In some cases, the sheath or introducer may be left in the insertion site. If so, the bedrest will be last until the sheath is removed. After the sheath is removed, you may be given a light meal.
You may feel the urge to urinate often because of the effects of the contrast dye and increased fluids. You will need to use a bedpan or urinal while on bed rest so that your affected leg or arm will not be bent.
After the specified period of bed rest has been completed, you may get out of bed. The nurse will help you the first time you get up, and will check your blood pressure while you are lying in bed, sitting, and standing. You should move slowly when getting up to avoid any dizziness from the long period of bed rest.
You may be given pain medication for pain or discomfort at the insertion site or from having to lie flat and still for a long time.
You will be encouraged to drink water and other fluids to help flush the contrast dye from your body.
You may go back your usual diet after the procedure, unless your doctor decides otherwise.
You will most likely spend the night in the hospital after your procedure. Depending on your condition and the results of your procedure, your stay may be longer. You will get detailed instructions for your discharge and recovery period.
At home
Once at home, monitor the insertion site for bleeding, unusual pain, swelling, abnormal discoloration, or temperature change. A small bruise is normal. If you notice a constant or large amount of blood at the site that cannot be contained with a small dressing, notify your doctor.
If your doctor used a closure device at your insertion site, you will be given specific information regarding the type of closure device that was used and how to take care of the site. There will be a small knot, or lump, under the skin at the site. This is normal. The knot should slowly disappear over a few weeks.
It will be important to keep the insertion site clean and dry. Your doctor will give you specific bathing instructions.
You may be advised not to participate in any strenuous activities. Your doctor will instruct you about when you can return to work and resume normal activities.
Notify your doctor if you have any of the following:
- Fever and/or chills
- Increased pain, redness, swelling, bleeding, or other drainage from the insertion site
- Coolness, numbness and/or tingling, or other changes in the affected arm or leg
- Chest pain/pressure, nausea and/or vomiting, profuse sweating, dizziness, and/or fainting
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- The risks and benefits of the test or procedure
- When and where you are to have the test or procedure and who will do it
- When and how will you get the results
- How much will you have to pay for the test or procedure
