What is a transesophageal echocardiogram?
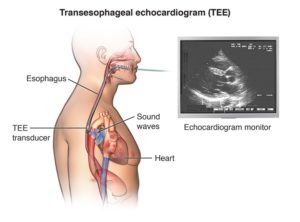 A transesophageal echocardiogram (TEE) uses echocardiography to assess how well the heart works. During the procedure, a transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or “echo” off of the heart structures. The transducer picks up the reflected waves and sends them to a computer. The computer displays the echoes as images of the heart walls and valves.
A transesophageal echocardiogram (TEE) uses echocardiography to assess how well the heart works. During the procedure, a transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or “echo” off of the heart structures. The transducer picks up the reflected waves and sends them to a computer. The computer displays the echoes as images of the heart walls and valves.
A transesophageal echocardiogram is done by inserting a probe with a transducer down the esophagus rather than placing the transducer on the chest in a transthoracic echocardiogram.
By inserting the transducer in the esophagus, TEE provides a clearer image of the heart because the sound waves do not have to pass through skin, muscle, or bone tissue. For example, being overweight or having certain lung diseases can interfere with images of the heart when the transducer is placed on the chest wall.
Certain conditions of the heart, such as mitral valve disorders, blood clots or masses inside the heart, a tear of the lining of the aorta and artificial heart valves, are better seen with TEE.
A TEE may use one or more of several special types of echocardiography, as listed below:
- M-mode echocardiography. This, the simplest type of echocardiography, produces an image that is similar to a tracing rather than an actual picture of heart structures. M-mode echo is useful for measuring heart structures, such as the heart’s pumping chambers, the size of the heart itself, and the thickness of the heart walls.
- Doppler echocardiography. This Doppler technique is used to assess blood flow through the heart’s chambers and valves. The amount of blood pumped out with each beat is an indication of the hearts functioning. Also, Doppler can detect abnormal blood flow within the heart, which can indicate a problem with one or more of the heart’s four valves, or with the heart’s walls.
- Color Doppler. Color Doppler is an enhanced form of Doppler echocardiography. With color Doppler, different colors are used to designate the direction of blood flow. This simplifies the interpretation of the Doppler technique.
- 2-D (two-dimensional) echocardiography. This technique is used to view the motion of the heart structures. A 2-D echo view appears cone-shaped on the monitor. It shows the real-time motion of the heart’s structures. This lets the doctor to see the various heart structures at work and evaluate them.
- 3-D (three-dimensional) echocardiography. This technique captures three-dimensional views of the heart structures with greater depth than 2-D echo. The live or “real time” images allow for a more accurate assessment of heart function by using measurements taken while the heart is beating.
Why might I need a transesophageal echocardiogram?
Transesophageal echocardiography may be done to evaluate signs and symptoms that may suggest:
- Atherosclerosis. This is a gradual clogging of the arteries by fatty materials and other substances in the blood stream. It happens over many years.
- Cardiomyopathy. This is an enlargement of the heart due to thickening or weakening of the heart muscle.
- Congenital heart disease. These defects in one or more heart structures occur during formation of the fetus. This includes ventricular septal defect (hole in the wall between the two lower chambers of the heart).
- Heart failure. A condition in which the heart muscle has become weakened to an extent that blood can’t be pumped efficiently. This can cause fluid buildup (congestion) in the blood vessels and lungs, and edema (swelling) of the feet, ankles, and other parts of the body.
- Aneurysm. This is a weakening and bulging of a part of the heart muscle or the aorta (the large artery that carries oxygenated blood out of the heart to the rest of the body).
- Heart valve disease. Malfunction of one or more of the heart valves that may block blood flow within the heart.
- Cardiac tumor. A tumor of the heart may occur on the outside surface of the heart, within one or more chambers of the heart , or within the muscle tissue of the heart.
- Pericarditis. This is an inflammation or infection of the sac that surrounds the heart.
- Infective endocarditis. This is an infection of the heart, usually affecting the heart valves.
Additional reasons for which a TEE may be done include:
- To assess the heart’s function and structures
- To evaluate the heart during open-heart surgery after procedures, such as coronary artery bypass or valve replacement or repair
- To evaluate the heart during non-cardiac surgery
There may be other reasons for your doctor to recommend a TEE.
What are the risks of a transesophageal echocardiogram?
Possible risks associated with a transesophageal echocardiogram include:
- Breathing problems
- Heart rhythm problems
- Infection
- Bleeding
- Injury to the mouth, throat or esophagus
If you have known problems of the esophagus, such as esophageal varices, esophageal obstruction, or radiation therapy to the area of the esophagus, you may not be able to have a TEE. Your doctor will evaluate you carefully before having the procedure.
If you are allergic to or sensitive to medications or latex , tell your doctor.
If you are pregnant or think you may be, tell your doctor.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
How do I get ready for a transesophageal echocardiogram?
- Your doctor will explain the procedure to you and offer you the chance to ask questions.
- You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
- You will need to fast for a certain period prior to the procedure. Your doctor will tell you how long to fast, whether for a few hours or overnight.
- If you are pregnant or think you may be, tell your doctor.
- Tell the doctor if you are allergic to or sensitive to medications, local anesthesia, or latex.
- Tell your doctor of all medications (prescription and over-the-counter) and herbal supplements that you are taking.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop some of these medications prior to the procedure.
- Your doctor may request a blood test prior to the procedure to determine how long it takes your blood to clot. Other blood tests may be done as well.
- Tell the doctor if you have heart valve disease, a congenital heart condition, or a history of endocarditis (infection of the heart valves).
- You may receive a sedative prior to the procedure to help you relax. If a sedative is given, you will need someone to drive you home afterwards.
- Based on your medical condition, your doctor may request other specific preparation.
What happens during a transesophageal echocardiogram?
A TEE may be done on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor’s practices.
Generally, a TEE follows this process:
- You will be asked to remove any jewelry or other objects that may interfere with the procedure. If you wear dentures or any oral prosthesis, they will be removed prior to the insertion of the TEE probe.
- If you are asked to remove clothing, you will be given a gown to wear.
- You will be asked to empty your bladder prior to the procedure.
- An intravenous (IV) line will be started in your hand or arm prior to the procedure for injection of medication and to administer IV fluids, if needed.
- You will lie on a table or bed, positioned on your left side. A pillow or wedge may be placed behind your back for support.
- You will be connected to an electrocardiogram (EKG) monitor that records the electrical activity of the heart and monitors the heart during the procedure using small, adhesive electrodes. Your vital signs (heart rate, blood pressure, breathing rate, and oxygenation level) will be monitored during the procedure.
- A local anesthetic spray will be applied to the back of the throat. This will numb the back of your throat to make passing the TEE probe more comfortable.
- You will receive a sedative medication in your IV before the procedure to help you relax.
- If indicated, oxygen will be given through nasal tubes.
- The room will be darkened so that the images on the echocardiogram monitor can be seen by the doctor.
- The TEE probe will be passed through your mouth and down your throat. You may be asked to swallow to help pass the probe.
- Once the probe is in the right place, the images are taken.
- After the necessary images are taken, the probe will be removed from your throat.
What happens after a transesophageal echocardiogram?
You will be moved to a recovery area, where nurses will monitor your heart rate, EKG, blood pressure, and oxygen levels.
When your gag reflex has returned, your vital signs are stable, and you are more alert, the EKG electrode pads, the oxygen probe, and the IV will be removed. You may get dressed.
You may feel weak, tired, or groggy for the rest of the day of the test. You should feel normal by the day after the procedure. Your throat may be sore for a few days after the procedure due to the insertion of the TEE probe.
If the procedure was done on an outpatient basis, you may be discharged home, unless your doctor determines that your condition requires further observation or hospital admission.
If you received sedation, you will need to have someone drive you home.
You may resume your usual diet and activities unless your doctor advises you differently.
Generally, there is no special type of care following a TEE. However, your doctor may give you other instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- The risks and benefits of the test or procedure
- When and where you are to have the test or procedure and who will do it
- When and how will you get the results
- How much will you have to pay for the test or procedure
